Welcome to our latest article on the relationship between TURP (transurethral resection of the prostate) and prostate cancer risk. In this section, we will explore the question: Can TURP spread prostate cancer?
Prostate cancer is a significant concern for men worldwide, with surgical methods like TURP being commonly used in its treatment. However, there have been concerns about the potential for cancer spread during this procedure. In this article, we will examine the available evidence and shed light on this topic.
Stay with us as we delve into the details of TURP, the risks involved, and its impact on prostate cancer treatment.
Key Takeaways:
- There is limited evidence suggesting tumor dissemination during a TURP procedure.
- Prostate cancer outcomes are similar in TURP and non-TURP treated patients.
- TURP does not increase the risk of cancer cells spreading beyond the prostate.
- Delayed radiation therapy after TURP can minimize potential complications.
- TURP does not increase morbidity following radical prostatectomy.
The Relationship Between TURP and Prostate Cancer
When it comes to the relationship between transurethral resection of the prostate (TURP) and prostate cancer, numerous studies have shed light on the subject. Contrary to popular misconceptions, there is no evidence to suggest a direct causality between TURP and the spread or progression of prostate cancer.
TURP is primarily performed as a surgical method to alleviate urinary symptoms caused by prostate enlargement, commonly known as benign prostatic hyperplasia. During the procedure, prostate tissue may be removed to relieve the obstruction, but this does not increase the risk of cancer cells spreading beyond the prostate.
It is important to understand that TURP targets the non-cancerous part of the prostate, aiming to improve the patient’s quality of life by alleviating urinary symptoms. Cancer cells are localized within the tumor, and TURP does not involve removal or disruption of the tumor itself, thereby minimizing the potential for cancer spread.
Studies have consistently shown no significant difference in cancer progression or prognosis between patients who undergo TURP and those who do not. The focus of TURP is solely on improving urinary function and reducing symptoms related to prostate enlargement.
Thus, if you have been diagnosed with prostate cancer and require TURP to address urinary symptoms, rest assured that the procedure will not exacerbate the cancer or impact the overall effectiveness of your prostate cancer treatment plan.
Potential Adverse Effects of TURP on Prostate Cancer Treatment
When considering the treatment of prostate cancer, one concern that arises is whether transurethral resection of the prostate (TURP) may have adverse effects on other forms of treatment such as radiation therapy or radical prostatectomy. It is important for patients and healthcare providers to understand the potential risks and complications associated with TURP in the context of prostate cancer management.
While TURP is a commonly performed surgical procedure to alleviate obstructive urinary symptoms caused by prostate enlargement, its impact on prostate cancer treatment is a matter of interest. Some studies suggest that TURP performed before radiation therapy may increase the risk of complications such as incontinence and bladder neck contracture. However, these risks can be minimized by implementing a waiting period of 6 to 8 weeks between TURP and radiation therapy.
Despite these concerns, there is no compelling evidence to indicate that TURP increases morbidity following a radical prostatectomy. In fact, TURP can be beneficial in select cases by addressing urinary symptoms and improving quality of life before undergoing a radical prostatectomy.
Risks of TURP in the Context of Radiation Therapy
When TURP is performed before radiation therapy, there are potential risks that need to be considered. These risks include:
- Incontinence: Some patients may experience urinary incontinence as a result of TURP. This can be temporary or permanent, depending on the individual case.
- Bladder neck contracture: TURP may cause scar tissue formation in the bladder neck, leading to urinary flow obstruction. This can be treated with additional surgical interventions if necessary.
- Delayed radiation treatment: The need for a waiting period between TURP and radiation therapy may result in a delay in initiating cancer treatment.
Precautions for Minimizing Complications
To minimize the potential complications associated with TURP and subsequent radiation therapy, healthcare providers may suggest the following precautions:
- Delaying radiation therapy: Implementing a waiting period of 6 to 8 weeks after TURP can allow for proper healing and minimize the risk of incontinence and bladder neck contracture.
- Close monitoring: Regular follow-up appointments with healthcare providers will ensure any post-TURP complications are identified and managed promptly.
- Individualized treatment approach: Each patient’s case must be evaluated individually to determine the most appropriate course of action for both TURP and radiation therapy.
It is important for patients to have open and honest discussions with their healthcare providers about their treatment options, including the potential risks and benefits of TURP in relation to prostate cancer management. By considering all available information and making informed decisions, patients can work together with their healthcare team to develop the most suitable treatment plan for their specific needs.
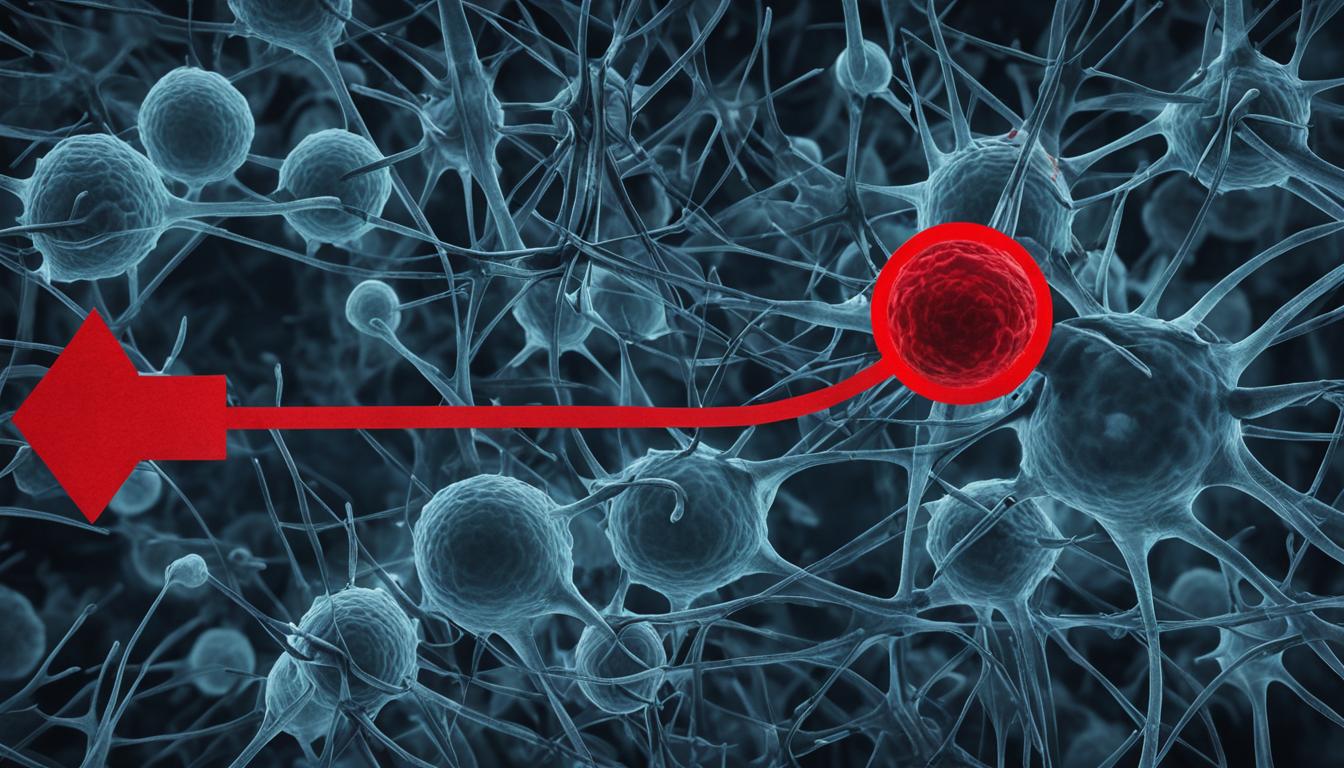
Mechanisms of Cancer Spread during Invasive Procedures
When it comes to invasive procedures for prostate cancer, there are two proposed mechanisms by which cancer cells may spread: direct implantation and release of tumor cells. Direct implantation refers to the transfer of cancer cells from invasive instruments during procedures such as biopsy, surgery, or brachytherapy. On the other hand, the release of tumor cells occurs when cancer cells enter the bloodstream or lymphatic system, potentially spreading to other parts of the body.
It is important to note, however, that only specific types of prostate cancer cells have the ability to spread through these mechanisms. The most prevalent types of prostate cancer are confined to the prostate and are unable to survive outside of it. Therefore, the risk of tumor dissemination and implantation during invasive procedures is relatively low for the majority of prostate cancer cases.
To better understand the concept, let’s take a closer look at these two mechanisms:
1. Direct Implantation
“Direct implantation refers to the transfer of cancer cells from invasive instruments during procedures such as biopsy, surgery, or brachytherapy.”
During invasive procedures, there is a slight risk of cancer cells being introduced to new sites within the body through the direct contact of instruments with the tumor. This can occur if the instruments inadvertently come into contact with cancerous tissue during the procedure. While this risk exists, it is important to note that precautions are taken to minimize the likelihood of implantation, such as ensuring proper sterilization and handling of instruments.
2. Release of Tumor Cells
“The release of tumor cells occurs when cancer cells enter the bloodstream or lymphatic system, potentially spreading to other parts of the body.”
Another mechanism by which cancer cells can potentially spread during invasive procedures is through the release of tumor cells into the bloodstream or lymphatic system. This can happen when procedures like biopsy, surgery, or brachytherapy disrupt the tumor, allowing cancer cells to enter the circulation. However, it is important to note that not all prostate cancer cells have the ability to survive and thrive outside of the prostate. Therefore, the risk of widespread dissemination through this mechanism is limited to specific types of prostate cancer.
The overall risk of tumor dissemination and implantation during invasive procedures for prostate cancer is relatively low. Healthcare professionals take precautions to minimize these risks and ensure patient safety. While rare occurrences of cancer spread have been reported, they are isolated cases and not representative of the general outcomes of invasive procedures.
| Mechanism | Risk Level |
|---|---|
| Direct Implantation | Low |
| Release of Tumor Cells | Low, limited to specific types of prostate cancer |
It is important for patients to discuss any concerns about cancer spread with their healthcare providers. While the risk is low, healthcare professionals can provide personalized information and guidance based on individual circumstances. Understanding the mechanisms of cancer spread during invasive procedures can help alleviate any anxieties and allow patients to make informed decisions about their prostate cancer treatment.
Risks and Complications of Invasive Procedures for Prostate Cancer
When it comes to treating prostate cancer, various invasive procedures can be used, such as biopsies, surgeries, and brachytherapy. While these procedures have high cure rates and are effective in treating prostate cancer, it’s important to be aware of the potential risks and complications they may carry.
Although rare, there have been isolated case reports of cancer spread during invasive procedures. However, the occurrence of such cases is minimal. It’s essential to understand that these procedures are performed by experienced healthcare professionals who prioritize patient safety and follow meticulous protocols to minimize any potential risks.
Here are some potential risks and complications associated with invasive procedures for prostate cancer:
- Needle track seeding: In some cases, the biopsy needle may cause cancer cells to spread along the needle’s path.
- Positive surgical margins: During surgery, it’s crucial to remove the entire prostate gland without leaving any cancerous tissue behind. Positive surgical margins refer to the presence of cancer cells at the edges of the removed tissue.
- Tumor cell release into systemic circulation: In some instances, invasive procedures may lead to the release of cancer cells into the bloodstream or lymphatic system, potentially allowing them to travel to other parts of the body.
Although these risks exist, it’s important to note that they are not common occurrences. The benefits of these invasive procedures, including accurate diagnosis, effective treatment, and improved quality of life, often outweigh the potential risks. Healthcare providers work closely with patients to assess individual risks and benefits and devise personalized treatment plans.
Remember, the ultimate goal of invasive procedures for prostate cancer is to eliminate or manage the cancer effectively. While there may be risks involved, the overall success rates of these procedures in treating prostate cancer are high.
“Invasive procedures like biopsies, surgeries, and brachytherapy have proven to be effective in treating prostate cancer and are associated with high cure rates.”

The Importance of Surgeon Experience in Minimizing Cancer Spread
When it comes to invasive procedures for prostate cancer, surgeon experience plays a crucial role in minimizing the risk of cancer spread. Skilled and experienced surgeons understand the importance of precision and meticulousness in these delicate procedures, aiming to avoid cutting into tumors and ensuring complete removal of the prostate.
One technique that experienced surgeons employ is nerve-sparing surgery, which aims to preserve the nerves surrounding the prostate, minimizing the risk of nerve damage and potential cancer spread. Additionally, careful anastomosis, the technique used to stitch the bladder and urethra back together after prostate removal, is performed with utmost attention to detail to minimize the risk of complications and cancer dissemination.
Choosing a skilled and experienced surgeon is therefore vital when undergoing surgical interventions for prostate cancer. By entrusting your care to a knowledgeable and experienced professional, you can have confidence in their ability to minimize the potential for cancer spread and optimize your treatment outcome.

Expertise in Action: Dr. Emily Roberts
“As a highly experienced urologist specializing in prostate cancer surgery, my goal is to provide the best possible outcomes for my patients. With years of training and expertise, I employ the most advanced surgical techniques to minimize the risk of cancer spread during invasive procedures. By focusing on precision and meticulousness, I strive to ensure that my patients receive the highest quality of care and achieve favorable treatment outcomes.” – Dr. Emily Roberts, Urologist
Benefits of Surgeon Experience
The benefits of choosing an experienced surgeon for prostate cancer surgery are manifold:
- Minimization of cancer spread: Surgeon experience greatly reduces the risk of cancer cells spreading beyond the prostate, ensuring a more localized cancer treatment approach.
- Optimized treatment outcomes: Skilled surgeons are adept at complete prostate removal and minimizing complications, leading to better treatment outcomes.
- Reduced risks of post-surgical complications: Surgeons with extensive experience are well-versed in managing potential post-surgical complications, such as incontinence and bladder neck contracture.
- Nerve preservation: With a focus on nerve-sparing techniques, experienced surgeons strive to preserve sexual and urinary function, enhancing quality of life post-surgery.
By prioritizing surgeon experience and seeking out highly skilled professionals, patients can mitigate the risk of cancer spread during invasive procedures and optimize their overall treatment experience.
Conclusion
In conclusion, the available evidence indicates that TURP does not significantly increase the risk of cancer spread or affect the outcomes of prostate cancer treatment. While isolated cases of cancer dissemination during invasive procedures may occur, they are uncommon. Factors such as surgeon experience and appropriate treatment planning can further reduce the chances of cancer spread. Therefore, it is crucial for patients to have open discussions with their healthcare providers regarding the potential risks and benefits of invasive procedures to make informed decisions about their treatment.
Prostate cancer is a complex condition, and each patient’s situation is unique. It is important to consider all available treatment options and consult with experts to determine the most appropriate course of action. TURP remains a valuable procedure for relieving urinary symptoms caused by prostate enlargement, and its risks in relation to cancer spread are minimal.
While prostate cancer treatment can be daunting, understanding the available evidence and consulting with knowledgeable professionals can help alleviate concerns and guide patients towards the best treatment approach. The field of prostate cancer research and treatment continues to advance, and ongoing research will provide further insights into optimizing patient outcomes while minimizing potential complications.
FAQ
Can transurethral resection of the prostate (TURP) spread prostate cancer?
No, studies have shown that there is no direct causality between TURP and the spread or progression of prostate cancer. TURP is primarily performed to relieve urinary symptoms caused by prostate enlargement and does not increase the risk of cancer cells spreading beyond the prostate.
What is the relationship between TURP and prostate cancer?
TURP is not a treatment for prostate cancer but is performed to alleviate urinary symptoms caused by prostate enlargement. While TURP involves the removal of prostate tissue, it does not increase the risk of cancer spread or progression.
What are the potential adverse effects of TURP on prostate cancer treatment?
There is concern that TURP may increase the morbidity of radiation therapy or radical prostatectomy. However, studies suggest that delaying radiation treatment for 6 to 8 weeks after TURP can help minimize potential complications. Additionally, TURP does not increase morbidity following a radical prostatectomy.
How do invasive procedures contribute to cancer spread?
There are two proposed mechanisms by which invasive procedures may facilitate the spread of cancer cells: direct implantation from invasive instruments and the release of tumor cells into the bloodstream or lymph. However, only specific types of prostate cancer cells are capable of spreading through these mechanisms, and the most prevalent types of prostate cancer cannot survive outside of the prostate.
What are the risks and complications of invasive procedures for prostate cancer?
Invasive procedures such as biopsies, surgeries (including TURP), and brachytherapy carry the risks of needle track seeding, positive surgical margins, and the potential for tumor cell release into systemic circulation. However, these procedures have high cure rates and generally do not result in significant cancer spread.
How does surgeon experience minimize the risk of cancer spread during invasive procedures?
Experienced surgeons aim to avoid cutting into tumors and ensure complete removal of the prostate. Techniques such as nerve-sparing surgery and careful anastomosis can also help reduce the risk of cancer spread. Choosing a skilled and experienced surgeon is paramount in minimizing the potential for cancer spread during surgical interventions for prostate cancer.
What is the conclusion regarding TURP and prostate cancer risk?
The available evidence suggests that TURP does not significantly increase the risk of cancer spread or impact the outcomes of prostate cancer treatment. While rare occurrences of cancer spread during invasive procedures have been reported, they are isolated cases. Surgeon experience and appropriate treatment planning can further minimize the potential for cancer spread. It is important for patients to discuss the potential risks and benefits of invasive procedures with their healthcare providers to make informed treatment decisions.
Can TURP Treatment for Prostate Cancer Increase the Risk of Spread?
The claim linking anal sex and prostate cancer facts to an increased risk of spread following TURP treatment for prostate cancer is not supported by scientific evidence. TURP is generally considered safe and effective for managing prostate cancer symptoms. Patients should consult their healthcare provider for accurate information.