At first glance, it may seem that hemorrhoids and prostatitis have little in common. However, there may be a potential connection between these two conditions. Hemorrhoids are swollen veins in and around the anus, while prostatitis is the inflammation of the prostate gland. Although it is not very common, understanding the possible relationship between hemorrhoids and prostatitis is important to ensure proper management and care. Let’s explore the facts.
Key Takeaways:
- Hemorrhoids and prostatitis are inflammatory conditions that may have a potential connection.
- Hemorrhoids are swollen veins in the anus, while prostatitis is the inflammation of the prostate gland.
- While it is not very common, the interaction between the blood vessels, nerves, and lymph vessels in the anorectum and prostate could potentially contribute to prostatitis in some cases of hemorrhoids.
- However, other risk factors and causes such as bacterial infections or urinary tract issues are more commonly associated with prostatitis.
- If you experience symptoms of hemorrhoids or prostatitis, it is always recommended to consult a healthcare professional for accurate diagnosis and appropriate treatment.
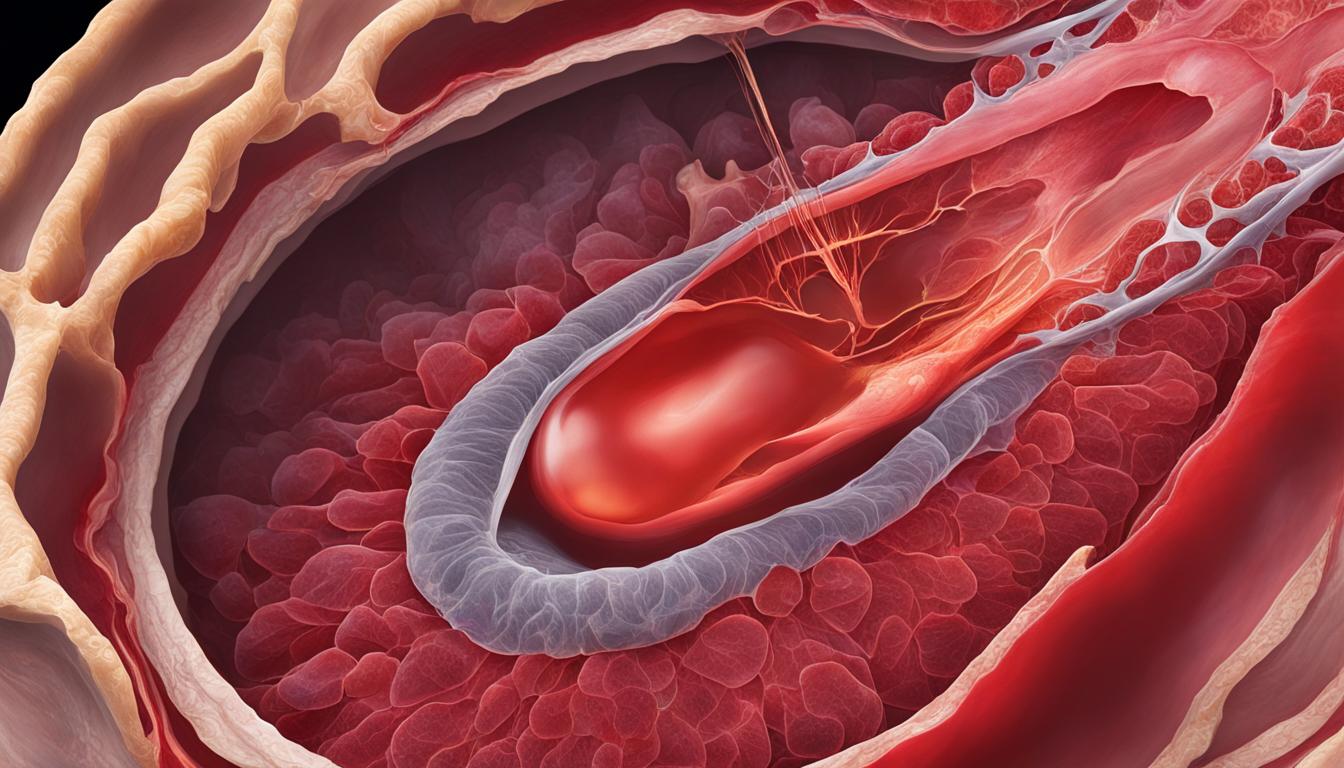
Understanding Hemorrhoids
Hemorrhoids, also known as piles, are a common condition characterized by swollen veins in and around the anus. They can cause discomfort, pain, and bleeding, affecting both men and women of all ages.
There are different types of hemorrhoids that can occur:
- External hemorrhoids: These develop outside the anus and can be felt as lumps.
- Thrombosed hemorrhoids: These occur when blood clots form in the external hemorrhoids, causing severe pain and swelling.
- Internal hemorrhoids: These are located inside the rectum and are typically painless but may cause bleeding.
- Prolapsed hemorrhoids: These occur when internal hemorrhoids protrude outside the anus and may need to be pushed back in manually.
The causes of hemorrhoids can vary, but they often develop due to increased pressure on the veins in the rectal area. Common risk factors include:
- Prolonged straining during bowel movements
- Being overweight or obese
- Having a low-fiber diet
- Experiencing recurrent constipation or diarrhea
- Lifting heavy objects frequently
- Spending prolonged periods of time sitting on the toilet
Hemorrhoids can manifest with various symptoms, such as:
- Blood in the stool or on toilet paper
- Itching or irritation in the anal area
- Lumps near the anus
- Discomfort or pain during bowel movements
- Rectal bleeding
When it comes to treating hemorrhoids, there are several options available depending on the severity of the condition. Mild cases can often be managed with home remedies, which include:
- Increasing water intake and consuming high-fiber meals to soften the stool
- Taking over-the-counter medications to relieve pain and reduce inflammation
- Applying topical creams or ointments to soothe itching and discomfort
For more severe or persistent hemorrhoids, procedural or clinic-based treatments may be necessary. These can include:
- Rubber band ligation: A small rubber band is placed at the base of the hemorrhoid to cut off its blood supply, causing it to shrink and fall off.
- Electrocoagulation: Heat is used to cauterize and shrink the hemorrhoid.
- Infrared coagulation: Infrared light is used to coagulate the blood vessels, causing the hemorrhoid to shrink.
- Sclerotherapy: A chemical solution is injected into the hemorrhoid to shrink it.
- Hemorrhoidectomy: Surgical removal of the hemorrhoid is performed under anesthesia.
- Hemorrhoid stapling: This procedure uses a special stapling device to block the blood flow to the hemorrhoid, causing it to shrink.
Prevention is key when it comes to managing and reducing the risk of developing hemorrhoids. Some preventive measures include:
- Visiting the toilet when the body urges to prevent constipation
- Avoiding pushing too hard or straining during bowel movements
- Avoiding prolonged periods of time sitting on the toilet
- Engaging in regular exercise to promote healthy digestion and prevent constipation
- Maintaining a healthy weight and consuming a high-fiber diet
Hemorrhoids can cause discomfort and affect your daily life, but with the right knowledge and treatment, they can be managed effectively. If you are experiencing persistent symptoms or have concerns about hemorrhoids, it is recommended to consult a healthcare professional for accurate diagnosis and appropriate treatment options.
Understanding Prostatitis
Prostatitis is the inflammation of the prostate gland, which can cause various symptoms that can significantly impact a man’s quality of life. The symptoms of prostatitis may include:
- Frequent urge to urinate
- Painful urination
- Rectal pain or pressure
- Fever and chills
There are different types of prostatitis, each with its own characteristics:
- Chronic prostatitis
- Acute bacterial prostatitis
- Chronic bacterial prostatitis
- Asymptomatic inflammatory prostatitis
The exact cause of prostatitis is often unknown. However, it can be caused by various factors, including:
- Bacterial infection from the rectum or infected urine
- Abnormal urinary tract anatomy
- Bladder or urinary tract infections
- Swollen prostate
- Procedures that expose the urethra to catheter or scope
- Injury to the anorectal region
When it comes to treatment options for prostatitis, it depends on the type and severity of the condition. Some common treatment options include:
- Antibiotics to treat bacterial infections
- Muscle relaxers to ease pain and discomfort
- Warm baths to help relax the prostate and relieve symptoms
- Prostate massage to promote drainage and relieve pain
- Pain medications to manage discomfort
The Importance of Seeking Medical Attention
If you experience any symptoms of prostatitis or suspect you may have the condition, it is essential to seek medical attention. A healthcare professional can accurately diagnose your condition and recommend the most appropriate treatment options for your specific situation.
| Type of Prostatitis | Symptoms | Treatment Options |
|---|---|---|
| Chronic Prostatitis | Includes symptoms such as pelvic pain, frequent urination, and discomfort during ejaculation. | Treatment options may include antibiotics, alpha-blockers, physical therapy, and lifestyle changes. |
| Acute Bacterial Prostatitis | Characterized by sudden onset symptoms such as fever, chills, and severe pain in the lower abdomen or pelvic area. | Immediate medical attention is necessary. Treatment typically involves antibiotics and pain management. |
| Chronic Bacterial Prostatitis | Similar symptoms to chronic prostatitis but caused by recurrent bacterial infections. | Treatment involves long-term antibiotic therapy and other measures to manage symptoms. |
| Asymptomatic Inflammatory Prostatitis | Typically does not present with noticeable symptoms and is often diagnosed incidentally during prostate exams. | No specific treatment is usually required. Regular monitoring may be advised. |
It’s important to note that prostatitis can have a significant impact on a man’s physical and emotional well-being. Seeking timely medical attention and following the recommended treatment plan can help manage symptoms and improve overall quality of life.
The Connection between Hemorrhoids and Prostatitis
While there may be a connection between hemorrhoids and prostatitis, it is not very common. The blood vessels, nerves, and lymph vessels of the prostate and anorectum interact, and if pathogens spread through these vessels, hemorrhoids may lead to prostatitis. However, the chances of this happening are slim. It is important to note that other risk factors and causes, such as bacterial infections or urinary tract issues, are more commonly associated with prostatitis.
Understanding the Relationship
In rare cases, the inflammation caused by hemorrhoids can spread to the prostate gland, leading to prostatitis. This occurs when pathogens from the hemorrhoids, such as bacteria or viruses, enter the bloodstream or lymphatic system, causing an infection in the prostate. However, it’s essential to understand that this occurrence is not the primary cause of prostatitis. Other risk factors, like bacterial infections or urinary tract issues, are more commonly associated with prostatitis.
“While it is possible for hemorrhoids to cause prostatitis, it is not a common scenario. Prostatitis is usually caused by bacterial infections, urinary tract issues, or other underlying factors.”
It’s crucial to approach the connection between hemorrhoids and prostatitis with caution. While the two conditions share some anatomical proximity, the likelihood of hemorrhoids directly causing prostatitis is low. The primary causes of prostatitis are often unrelated to hemorrhoids, such as bacterial infections or urinary tract issues.

Risk Factors for Prostatitis
Prostatitis can be caused by various factors, including:
- Bacterial infections
- Urinary tract issues
- Abnormal urinary tract anatomy
- Prostate enlargement or swelling
- Injuries to the anorectal region
- Exposure to catheter or scope
| Risk Factors | Description |
|---|---|
| Bacterial infections | Infections caused by bacteria entering the urinary tract or rectum. |
| Urinary tract issues | Problems like bladder or urinary tract infections that can lead to prostatitis. |
| Abnormal urinary tract anatomy | Anatomical issues that can increase the risk of prostatitis. |
| Prostate enlargement or swelling | An enlarged or swollen prostate gland can contribute to prostatitis. |
| Injuries to the anorectal region | Injuries to the area around the anus and rectum can cause prostatitis. |
| Exposure to catheter or scope | Medical procedures that involve inserting a catheter or scope can introduce bacteria, leading to prostatitis. |
As we can see, the risk factors that commonly cause prostatitis are not directly related to hemorrhoids. Therefore, it is important to understand that the connection between hemorrhoids and prostatitis is not prevalent, and prostatitis is typically caused by other underlying factors.
Conclusion
In summary, while there is a possible connection between hemorrhoids and prostatitis, it is not a common occurrence. Hemorrhoids are characterized by swollen veins in and around the anus, while prostatitis is the inflammation of the prostate gland. It is crucial to have a comprehensive understanding of the causes, symptoms, and treatment options for both conditions in order to effectively manage and provide care.
If you experience persistent or worsening symptoms, it is highly recommended to seek the expertise of a healthcare professional for accurate diagnosis and appropriate treatment. Remember, prevention plays a vital role in reducing the risk of developing hemorrhoids or prostatitis. Adopting a healthy lifestyle, including a balanced diet and practicing good hygiene, can help safeguard against these conditions.
By staying informed and proactive, individuals can take charge of their well-being and make informed decisions regarding their health. Prioritize self-care, and consult a medical expert for personalized guidance. With proper knowledge and vigilance, we can maintain optimal health and minimize the impact of any potential health concerns.
FAQ
Can hemorrhoids cause prostatitis?
While there may be a possible connection between hemorrhoids and prostatitis, it is not a common scenario. Hemorrhoids are swollen veins in and around the anus, while prostatitis is the inflammation of the prostate gland. Understanding the causes, symptoms, and treatment options for both conditions is important for proper management and care.
What are the types of hemorrhoids?
There are different types of hemorrhoids, including external hemorrhoids, thrombosed hemorrhoids, internal hemorrhoids, and prolapsed hemorrhoids. Each type has distinct characteristics and may require different treatment approaches. It is best to consult a healthcare professional for accurate diagnosis and appropriate treatment.
What are the causes of hemorrhoids?
Hemorrhoids are often caused by straining during bowel movements, but other risk factors include being overweight, having a low-fiber diet, recurrent constipation or diarrhea, lifting heavy objects, and spending prolonged periods of time on the toilet. Understanding these causes can help in adopting preventive measures and promoting good bowel habits.
What are the symptoms of hemorrhoids?
Symptoms of hemorrhoids may include blood in the stool or on toilet paper, itching, lumps near the anus, and rectal bleeding. It is important to note that these symptoms can also be indicative of other conditions, so consulting a healthcare professional for an accurate diagnosis is essential.
How are hemorrhoids treated?
Treatment options for hemorrhoids range from home remedies such as increasing water intake and consuming high-fiber meals to procedural or clinic-based treatments like rubber band ligation, electrocoagulation, infrared coagulation, sclerotherapy, hemorrhoidectomy, and hemorrhoid stapling. The choice of treatment depends on the severity and type of hemorrhoids. It is advisable to consult a healthcare professional for personalized treatment recommendations.
What are the types of prostatitis?
There are different types of prostatitis, including chronic prostatitis, acute bacterial prostatitis, chronic bacterial prostatitis, and asymptomatic inflammatory prostatitis. Each type has different underlying causes and requires specific treatment approaches. It is important to consult a healthcare professional for an accurate diagnosis and appropriate treatment.
What are the causes of prostatitis?
The exact cause of prostatitis is often unknown, but it can be caused by bacterial infection from the rectum or infected urine. Other risk factors for prostatitis include abnormal urinary tract anatomy, bladder or urinary tract infections, swollen prostate, procedures that expose the urethra to catheter or scope, and injury to the anorectal region. Understanding these causes can help in preventing and managing prostatitis.
What are the symptoms of prostatitis?
Symptoms of prostatitis may include frequent urge to urinate, painful urination, rectal pain or pressure, fever, and chills. However, the severity and presentation of symptoms can vary depending on the type of prostatitis. It is crucial to seek medical attention for an accurate diagnosis and appropriate treatment.
How is prostatitis treated?
Treatment options for prostatitis depend on the type and severity of the condition and may include antibiotics, muscle relaxers, warm baths, prostate massage, and pain medications. The choice of treatment is usually personalized based on the individual’s symptoms and medical history. Consulting a healthcare professional is crucial for appropriate management and care.
Is there a connection between hemorrhoids and prostatitis?
While there may be a connection between hemorrhoids and prostatitis, it is not very common. The blood vessels, nerves, and lymph vessels of the prostate and anorectum interact, and if pathogens spread through these vessels, hemorrhoids may lead to prostatitis. However, the chances of this happening are slim. Other risk factors and causes, such as bacterial infections or urinary tract issues, are more commonly associated with prostatitis.
Can Using Sleep Aids for Enlarged Prostate Lead to Hemorrhoids?
Using natural sleep aids for enlarged prostate may lead to Hemorrhoids. Certain over-the-counter medications can relax the muscles in the rectum, which can contribute to the formation of hemorrhoids. It’s important to consult with a healthcare professional before using any sleep aids to ensure they are safe for your condition.